If you live in Arizona, you’ve probably heard of Valley fever.
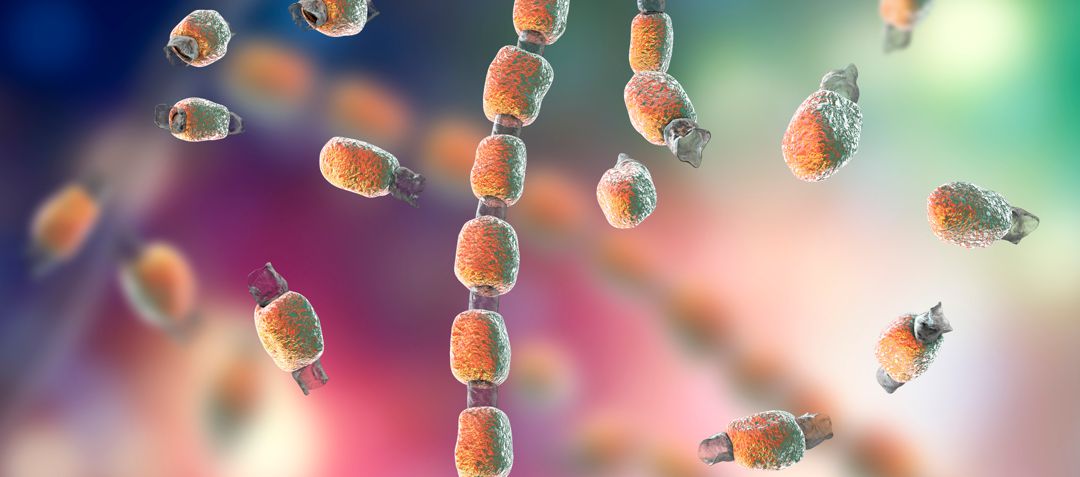
It is caused by a fungus – coccidioides – that grows in the soil of places with low rainfall, hot summers and mild winters, making Arizona and other Southwestern states a hot spot for the condition. In fact, most Valley fever cases reported to the Centers for Disease Control and Prevention come from Arizona or California.
 If you’re not familiar with Valley fever, here is some helpful information on symptoms, treatment and prevention from Dr. Sean Elliott, a pediatric infectious disease specialist at TMCOne.
If you’re not familiar with Valley fever, here is some helpful information on symptoms, treatment and prevention from Dr. Sean Elliott, a pediatric infectious disease specialist at TMCOne.
What are the symptoms of Valley fever?
Some 60% of Valley fever patients are asymptomatic, meaning they don’t experience any symptoms at all. Another 35% have flu-like symptoms such as low-grade fevers, malaise, achy muscles and headaches. The remaining 5% with severe Valley fever will have higher fevers, chest pain, cough and, sometimes, low blood pressure.
“Many patients, even those with mild symptoms, will experience night sweats,” Dr. Elliott said. “We’re talking the kind where one needs to dry out the pillow and the bedsheets in the morning. Many will also experience achy joints. In fact, Valley fever has been called ‘desert rheumatism’ because it causes small joints such as hands, wrists, feet and ankles to be achy.”
Some patients will develop a hive-like rash and red nodules on the lower legs over the shins. “Such people are having a hyper-immune response to the fungus causing Valley fever,” Dr. Elliott said.
When should you see a doctor?
Those with high fevers, severe cough or difficulty breathing, or losing weight from anorexia or malaise should see their doctor.
“Practically speaking, many patients seek medical care for prolonged fevers and night sweats, or for the rash, which can be quite striking,” Dr. Elliott said.
How do you get Valley fever in the first place? Is it contagious?
Valley fever is contracted by inhaling the spores in the air. It is typically associated with the dust in the air and seasonal winds. Those working in occupations such as construction, excavation, agriculture, archaeological digging or other fields that disturb the soil may be at increased risk of exposure.
It is not contagious from human to human.
How can you prevent getting Valley fever?
Because of how one contracts Valley fever, it can be hard to avoid. However, you can limit your exposure to the outdoors during windy times.
Who is at risk for severe disease?
Everyone who lives and travels in an area with Valley fever is at risk for getting the disease. However, being part of one of the following may increase your risk of developing severe disease:
- People with weakened immune systems such as organ transplant patients, Hodgkin’s disease patients, HIV/AIDS patients and people taking corticosteroids or certain types of drugs for autoimmune diseases or chemotherapy.
- African Americans and Filipinos are not more likely to get Valley fever, but, if they do get it, they have a higher risk of severe disease. Experts are not sure why this happens, but it might be because of genetic differences.
- People with diabetes are at higher risk of developing severe or chronic pneumonia. Diabetics with better controlled sugar levels may have less severe disease.
- Pregnant women are at greater risk of getting chronic or disseminated Valley fever, especially during the third trimester and right after giving birth.
How is Valley fever treated?
Most people do not need treatment because their immune system handles it. Those with risk factors for severe disease, such as certain ethnicities (Black, Filipino or Marshallese), people with immunodeficiency diseases or who are on immunosuppressive medications, are more likely to be treated with fluconazole, an antifungal medication, than someone without these risk factors.
—
If you have symptoms of Valley fever, speak to your primary care provider about treatment options. If you need a primary care provider, find one at TMCOne.com.